Which Tool Is Often Used By Case Managers?
The case management knowledge framework consists of what instance managers need to know (knowledge, skills, and competencies) to finer intendance for clients and their support systems. It includes two primary elements:
- A ix-stage Case Management Process
- Half-dozen essential knowledge domains (previously seven domains that have been updated based on findings of the case manager's part and function report CCMC recently conducted)
These elements are applicable in any care or practice setting and for the diverse healthcare professionals who presume the case director's function and/or those directly or indirectly involved in the field.
Definition of Instance Management
At that place is no one standardized or nationally recognized or even widely accepted definition of case management. An Internet search for the definition of the term case direction volition consequence in thousands of references. Such results are confusing for case managers and others who are interested in case management practice. Y'all may be unable to discern which definition is nigh apparent or relevant.
Despite the large search consequence, experts would agree that at that place are no more than xx or and so definitions of instance direction considered appropriate. These definitions are available in peer-reviewed professional case management literature or on Web sites and in other formal documents of example management (or example management-related) organizations, societies, and government or nongovernment agencies. The Instance Management Knowledge Framework

View larger epitome
So that you do not get confused as you read materials in the Committee for Case Manager Certification'southward (CCMC) CMBOK®, the good contributors who adult the example direction cognition framework in 2009 decided to employ the Committee'southward definition of case management available at that time to guide their work. (Notation that the definition below has since been updated to reflect current appropriate data promulgated by CCMC.)
 "Example management is a professional person and collaborative procedure that assesses, plans, implements, coordinates, monitors, and evaluates the options and services required to meet an individual's wellness needs. Information technology uses communication and available resources to promote health, quality, and price-effective outcomes in support of the 'Triple Aim,' of improving the experience of care, improving the health of populations, and reducing per capita costs of wellness care." (CCMC, 2015, p. iv )
"Example management is a professional person and collaborative procedure that assesses, plans, implements, coordinates, monitors, and evaluates the options and services required to meet an individual's wellness needs. Information technology uses communication and available resources to promote health, quality, and price-effective outcomes in support of the 'Triple Aim,' of improving the experience of care, improving the health of populations, and reducing per capita costs of wellness care." (CCMC, 2015, p. iv )
Case Management Philosophy and Guiding Principles
Example management is a specialty practice within the health and human services profession. Everyone directly or indirectly involved in healthcare benefits when healthcare professionals and especially example managers appropriately manage, efficiently provide, and finer execute a client'due south intendance. The underlying guiding principles of case management services and practices of the CMBOK follow:
- Case management is non a profession unto itself. Rather, it is a cross-disciplinary and interdependent specialty do.
- Case management is a means for improving clients' health and promoting wellness and autonomy through advocacy, advice, education, identification of service resources, and facilitation of service.
- Example management is guided by the ethical principles of autonomy, beneficence, nonmaleficence, veracity, equity, and justice.
- Case managers come from different backgrounds within health and human services professions, including nursing, medicine, social work, rehabilitation counseling, workers' compensation, and mental and behavioral health.
- The master function of case managers is to abet for clients/support systems. Case managers understand the importance of achieving quality outcomes for their clients and commit to the appropriate use of resource and empowerment of clients in a style that is supportive and objective.
- Case managers' first duty is to their clients – analogous care that is safety, timely, effective, efficient, equitable, and client-centered.
- Example management services are offered according to the clients' benefits equally stipulated in their health insurance plans, where applicative.
- The Case Management Process is centered on clients/support systems. It is wholistic in its handling of clients' situations (east.thousand., addressing medical, physical, functional, emotional, fiscal, psychosocial, behavioral, spiritual, and other needs), as well as those of their support systems.
- The Case Management Process is adaptive to case managers' practice settings and the settings where clients receive health and human services.
- Case managers approach the provision of case-managed health and human services in a collaborative style. Professionals from within or beyond healthcare organizations (eastward.g., provider, employer, payor, and community agencies) and settings collaborate closely for the benefit of clients/support systems.
- The goals of case management are offset and foremost focused on improving the client's clinical, functional, emotional, and psychosocial status.
- The healthcare organizations for which case managers work may also do good from case direction services. They may realize lowered health claim costs (if payor-based), shorter lengths of stay (if acute care-based), or early on return to work and reduced absenteeism (if employer-based).
- All stakeholders benefit when clients reach their optimum level of wellness, self-intendance management, and functional capability. These stakeholders include the clients themselves, their support systems, and the healthcare delivery systems, including the providers of intendance, the employers, and the diverse payor sources.
- Case direction helps clients achieve wellness and autonomy through advocacy, comprehensive assessment, planning, communication, wellness education and engagement, resource management, service facilitation, and use of evidence-based guidelines or standards.
- Based on the cultural beliefs, values, and needs of clients/support systems, and in collaboration with all service providers (both healthcare professionals and paraprofessionals), case managers link clients/support systems with appropriate providers of intendance and resource throughout the continuum of health and human services and across various intendance settings. They do and so while ensuring that the intendance provided is condom, constructive, customer-centered, timely, efficient, and equitable. This approach achieves optimum value and desirable outcomes for all stakeholders.
- Case direction services are optimized when offered in a climate that allows direct, open, and honest communication and collaboration amid the case manager, the client/support system, the payor, the primary care provider (PCP), the specialty care provider (SCP), and all other service delivery professionals and paraprofessionals.
- Case managers heighten the case management services and their associated outcomes by maintaining clients' privacy, confidentiality, health, and condom through advancement and adherence to ethical, legal, accreditation, certification, and regulatory standards and guidelines, as advisable to the practice setting.
- Case managers must possess the education, skills, noesis, competencies, and experiences needed to effectively render advisable, condom, and quality services to their clients/back up systems.
- Instance managers must demonstrate a sense of commitment and obligation to maintain current knowledge, skills, and competencies. They too must disseminate their practice innovations and findings from research activities to the case direction community for the benefit of advancing the field of example management.
Main Terms
Many terms in the CMBOK take multiple meanings, and y'all may exist unclear about which meaning to utilise. You might likewise non translate the terms in the way the noesis developers – who are case management experts – thought of them.
To get the virtually out of the knowledge these experts have shared in the CMBOK, accept the time to review the following terms. Annotation that the literature may describe these terms somewhat differently; the descriptions shared herein clarify their utilise throughout the CMBOK.
Primary Terms Used in the CMBOK
| Term | Description |
|---|---|
| Client | The recipient of example direction as well as health and human being services. "This private can be a patient, beneficiary, injured worker, claimant, enrollee, member, higher student, resident, or health intendance consumer of any age group. In addition, [use of] the term client may also infer the inclusion of the customer'due south back up [system]" (CMSA, 2016, p. 32). Annotation: In the CMBOK, the term client is sometimes intended to include the customer'southward support system. |
| Client's support system | The person or persons identified by each private client to be straight or indirectly involved in the customer's care. Information technology "may include biological relatives [family unit members], a spouse, a partner, friends, neighbors, colleagues, a health care proxy, or whatever individual who supports the client [caregivers, volunteers, and clergy or spiritual advisors]" (CMSA, 2016, p. 32). |
| Caregiver | The person responsible for caring for a client in the dwelling house setting and can be a family member, friend, volunteer, or an assigned healthcare professional. |
| Instance managing director | The health and human services professional responsible for coordinating the overall care delivered to an private client or a group of clients, based on the client'southward wellness or human services issues, needs, and interests. |
| Case management program | (Too referred to as case management section.) An organized approach to the provision of case management services to clients and their support systems. The programme is usually described in terms of:
|
| Case Management Procedure | The process through which case managers provide wellness and human services to clients/support systems. The procedure consists of several phases that are iterative, cyclical, and recursive rather than linear and that are applied until clients' needs and interests are met. The phases of the process are:
|
| Case managment plan of intendance | A comprehensive programme of intendance for an individual client that describes:
|
| Payor | The person, agency, or organization that assumes responsibility for funding the health and man services and resource consumed past a customer. The payor may be the customer him/herself, a member of the client'due south support organisation, an employer, a authorities benefit program (e.chiliad., Medicare, Medicaid, or TriCare), a commercial insurance agency, or a charitable organisation. |
| Practice setting | (Also referred to every bit practice site, intendance setting, or piece of work setting.) The system or bureau at which example managers are employed and execute their roles and responsibilities. The practice of instance management extends across all settings of the health and human being services continuum. These may include but are not limited to payor, provider, government, employer, customs, contained/private, workers' compensation, or a client'south home environment. |
| Professional subject | Case managers' formal education, training, and specialization or professional person background that is necessary and prerequisite for consideration as health and human services practitioners. Also refers to the professional background – such as nursing, medicine, social piece of work, or rehabilitation – that case managers bring with them into the practice of case direction. |
| Knowledge domain | A drove of information topics associated with health and human services and related subjects. These topics are organized around common themes (domains) to grade high-level/abstruse concepts that are considered to be essential for effective and competent performance of instance managers. Examples of case direction knowledge domains are Quality and Outcomes Evaluation and Measurement, and Care Delivery and Reimbursement Methods. |
| Health | An individual's concrete, functional, mental, behavioral, emotional, psychosocial, and cognitive condition. It refers to the presence or absence of illness, disability, injury, or limitation that requires special management and resolution, including the utilise of health and human services-type interventions or resources. NOTE: Throughout the CMBOK, the term health implies all aspects of health every bit described in the main term, reflecting a wholistic view of the client'southward condition or situation. |
| Health and human services continuum | The range of intendance that matches the ongoing needs of clients every bit they are served over time by the Example Management Procedure and case managers. It includes the advisable levels and types of care – health, medical, fiscal, legal, psychosocial, and behavioral – across one or more intendance settings. The levels of care vary in complexity and intensity of healthcare services and resources, including individual providers, organizations, and agencies. Annotation: Throughout the CMBOK, the term healthcare refers to and incorporates "health and human services," reflecting the broader customs of professionals who serve clients and the continuum of services they provide. |
| Level of care | The intensity and effort of health and human services and intendance activities required to diagnose, treat, preserve, or maintain clients' wellness. Level of care may vary from least to most complex, least to most intense, or prevention and wellness to astute care and services. |
| Community services and resources | Healthcare programs that offering specific services and resources in a customs-based surround equally opposed to an institutional setting (i.e., outside the confines of healthcare facilities such as hospitals and nursing homes). These programs either are publicly or privately funded or are charitable in nature. |
| Do good programs | The sum of services offered by a health insurance plan, authorities agency, or employer to individuals based on some sort of an agreement betwixt the parties (east.g., employer and employee). Benefits vary based on the plan and may include doc and hospital services, prescriptions, dental and vision care, workers' compensation, long-term intendance, mental and behavioral wellness, disability and adventitious death, counseling, and other therapies such every bit chiropractic care. |
| Benefits | The type of health and human being services covered by a health insurance plan (sometimes referred to as health insurance benefits, health benefits, or benefits plan) and every bit agreed upon betwixt an insurance company and an individual enrollee or participant. The term also refers to the amount payable by an insurance company to a claimant or beneficiary under the claimant's specific coverage every bit stipulated in the health insurance program. |
| Services | Interventions, medical treatments, diagnostics, and other activities implemented to manage clients' weather condition, including health and human services problems and needs. The types of services implemented tin exist found in an private customer's example management plan of intendance, medical handling program, or other related documents equally applicable to the healthcare setting and the professional discipline of the provider of care and services. Notation: The term services is used generically in the CMBOK to include the various types of intendance and services described in a higher place. |
The Case Management Process
The Case Management Procedure consists of 9 phases through which case managers provide care to their clients: Screening, Assessing, Stratifying Gamble, Planning, Implementing (Intendance Coordination), Following-Upwards, Transitioning (Transitional Care), Communicating Post Transition, and Evaluating . The overall process is iterative, non-linear, and cyclical, its phases being revisited as necessary until the desired effect is achieved. It also is afflicted by the care setting where the client and client's support arrangement are beingness cared for and the practise setting of the case director.
Centering on a client and the customer'due south support system, the Case Management Process is wholistic in its approach to the management of the client's situation and that of the client's support system. It is adaptive both to the case manager's practice setting and to the healthcare setting in which the client receives services.
The High-Level Case Management Process
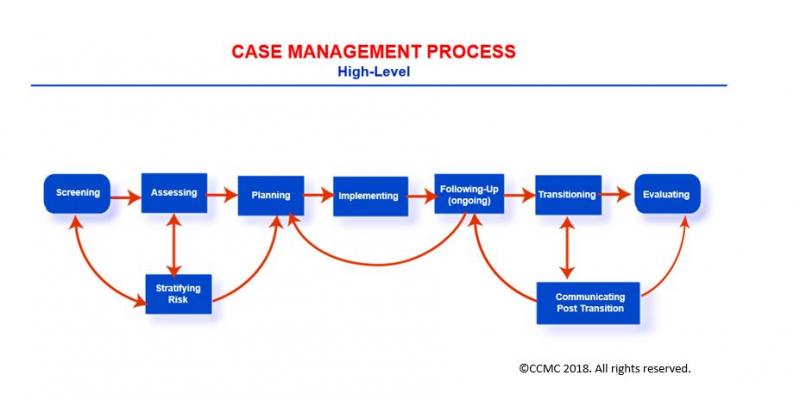
View larger image
Case managers navigate the phases of the procedure with careful consideration of the client's cultural behavior, interests, wishes, needs, and values. Past following the steps, they help clients/support systems to:
- Evaluate and understand the care options available to them
- Concord on their intendance goals and priorities
- Make up one's mind what is best to encounter their needs
- Institute action to achieve their goals and meet their interests/expectations
At the aforementioned time, case managers apply:
- Relevant country and federal laws
- Upstanding principles and standards such every bit the CCMC's Code of Professional Conduct for Case Managers with Standards, Rules, Procedures, and Penalties (CCMC, 2015), which applies to persons holding the CCM® credential
- Accreditation and regulatory standards
- Standards of intendance and do such as the CMSA Standards of Do for Case Management (CMSA, 2016)
- Show-based intendance or exercise guidelines
- Wellness insurance plan requirements and obligations as advisable
And at every phase of the Case Management Process, case managers provide vital documentation.
Customer Source
Before looking more than closely at the phases of the Case Management Process, first consider what triggers the procedure. You begin with the identification of a client. Without a client found to be in need of case direction services, y'all have no demand to launch the Case Management Process.
The client source – that is, how you, as case managers, come in contact with clients and/or their support systems – varies based on your practice setting.
Examples of Client Sources
| Care/Practice Setting | Highlights |
|---|---|
| Payor-based case manager | • May implement the Example Management Procedure for a client upon direct contact via the telephone past the customer/support system or upon referral from other professionals working for the payor system such as a medical manager, a claims adjuster, a clerical person, or a quality/functioning improvement specialist. |
| Astute care setting-based case director | May implement the Case Management Process for a client later referral from any of the healthcare squad members, including the md, primary nurse, social worker, consultant, specialist, therapist, dietitian, or manager. In some organizations, case managers may visit every new admission and deport a high-level review of the customer's state of affairs for the purpose of identifying whether the client would benefit from example management services. |
| Community care setting-based example managing director | May implement the Instance Direction Process for a client subsequently referral from the primary care provider or specialty intendance provider. In some instances, the case director may initiate the procedure based on a request from the customer/back up arrangement or based on a regulatory obligation such equally health home requirement for Medicare or Medicaid beneficiaries participating in an accountable care organization or federally qualified health care center. |
| Vocational rehabilitation or workers' bounty-based case managing director | May implement the Case Direction Process for a client after referral from the acute- or customs-based case director or other healthcare providers who have identified the client would do good from vocational rehabilitation case management services. In some instances, an employer may refer a client (e.g., on-the-job injured worker) for vocational rehabilitation as role of the return-to-work program of care. |
The Screening Phase
The Case Management Process: Screening
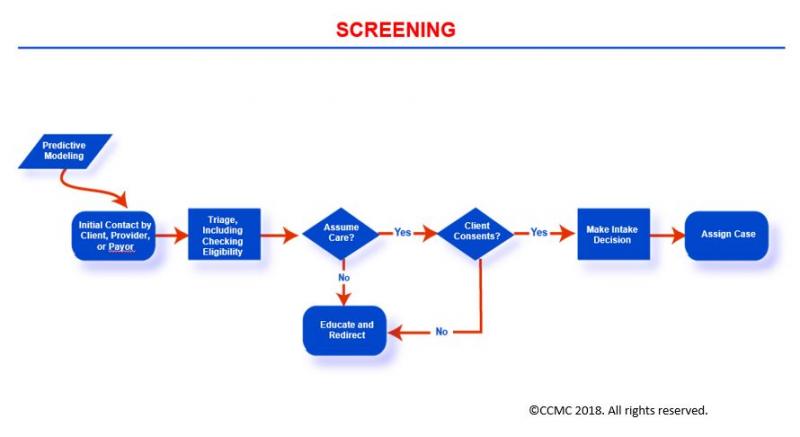
View larger image
Click here to view map fundamental for image
The Screening stage focuses on the review of primal information related to an individual's health situation in order to identify the need for wellness and human services (instance management services). Your objective of the screening equally the case manager is to determine if your client would benefit from such services.
Screening promotes early intervention and the achievement of desired outcomes. Key information about your customer/back up organization you gather during screening may include the following (to the extent bachelor):
- Risk stratification category or form
- Claims data
- Health services utilization
- By and current health condition
- Socioeconomic and financial status
- Health insurance coverage
- Home environment
- Prior services
- Physical, emotional, and cognitive functioning
- Psychosocial network and support system
- Self-care ability
The Assessing Phase
The Case Management Process: Assessing
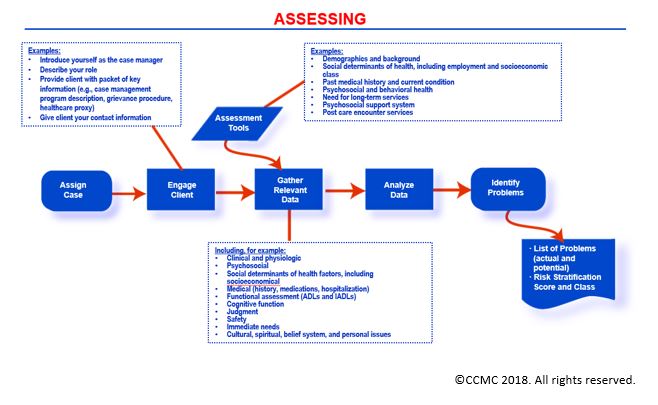
View larger image
Click hither to view map key for image
The Assessing stage involves the collection of information virtually a client's situation similar to those reviewed during screening, however to greater depth. The information yous collect virtually your customer/back up organization may include:
- Past and electric current wellness conditions
- Service utilization
- Socioeconomic and financial status
- Wellness insurance plan benefits and coverage
- Home status and safety
- Availability of prior services
- Physical, emotional, and cerebral performance
- Psychosocial network and back up organization
- Health appointment
- Self-care knowledge and ability
- Readiness for alter
You, the instance manager, have 3 primary objectives while assessing your customer/support system:
- Identifying the client's key problems to be addressed, besides every bit individual needs and interests
- Determining the expected intendance goals and target outcomes
- Developing a comprehensive instance management plan of care that addresses these problems and needs while allowing you lot to reach the care goals
You seek to confirm or update your client'due south adventure category based on the information you have gathered. You also may apply two primal strategies for your constructive data gathering. Using standardized cess tools and checklists, you:
- Get together the essential information telephonically or through face-to-face contact with your client, the client's back up system, and the clinicians involved in your customer'due south intendance.
- Collect necessary information through a review of current and past medical records, personal health records if bachelor, and advice with your client's employer, health insurance plan representative, and others every bit you deem advisable.
The Stratifying Hazard Phase
The Case Management Process: Stratifying Risk
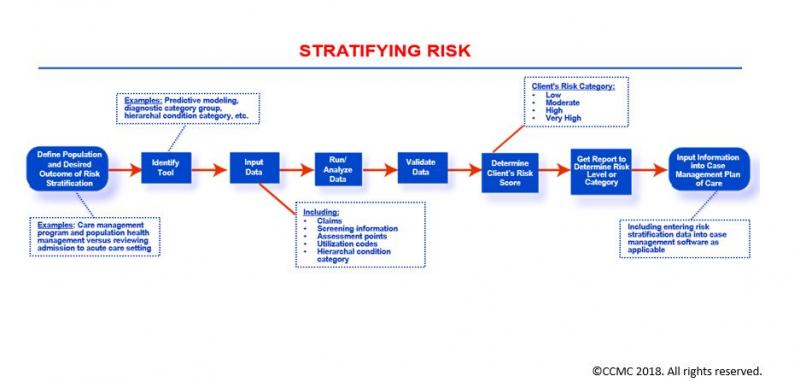
View larger image
Click hither to view map fundamental for image
The Stratifying Risk stage involves the classification of your client into one of three take a chance categories – low, moderate, and loftier – in order to determine the appropriate level of intervention based on your customer's situation and interests. This classification allows you to implement targeted risk category-based interventions and treatments that enhance your client's care interventions and outcomes.
When stratifying your client's run a risk, you equally the example manager complete a health run a risk assessment and biomedical screening based on specific gamble factors for your client.
Factors applied in a client's chance stratification may include:
- Presence and number of physical health conditions
- Medications intake: number and type (polypharmacy)
- Blood pressure
- Substance, alcohol, or tobacco use
- Nutrition and practise habits
- Blood saccharide level and lipids/cholesterol profile
- Emotional, mental, and behavioral health
- Admission to intendance and utilization of healthcare services (e.chiliad., emergency department visits or hospitalizations)
- Availability of psychosocial support organisation
- Gender, race, ethnicity, and age
- Socioeconomic and fiscal state of affairs (east.g., limited income, no insurance, underinsurance)
- Other risk factors depending on the risk assessment tool/model applied
In some organizations, such as those that are payor-based, stratifying risks may take identify prior to assessing the client. It also may be completed in an automated manner using conclusion support systems and based on claims data. In such situations, you as the case manager review the automatically generated take chances classifications and contact the client accordingly. You may also determine the need for contacting the client based on agreed-upon and nationally recognized algorithms, criteria and protocols.
It is common today to have a risk nomenclature organization that consists of four categories instead of 3. The 4th and additional level refers to a pocket-sized percentage of clients (i.e., no more than iii%) whose condition is extremely circuitous and requires an intensive amount of resource and the involvement of multiple healthcare providers with varied specialties. This group of patients is commonly described equally the "very high" risk category. When yous are managing this category of clients, you provide comprehensive case management services while interacting with such clients at a frequency that exceeds once per month – as high as perhaps weekly.
The Planning Phase
The Case Management Process: Planning
Click here to view map key for epitome
The Planning phase establishes specific objectives, intendance goals (curt- and long-term), and actions (treatments and services) necessary to meet a customer'south needs equally identified during the Screening and Assessing phases.
 You often consider the client'south risk nomenclature or category in the design of the client's plan of care.
You often consider the client'south risk nomenclature or category in the design of the client's plan of care.
During the Planning stage, you as the case manager develop a case management plan of intendance for your client that considers inputs and approvals of the client/back up arrangement and the client'southward healthcare providers. Your programme is activity-oriented, fourth dimension-specific, and multidisciplinary in nature. In this plan you address your customer's cocky-intendance management needs and intendance across the continuum, especially the services needed after a current episode of care; for example, care post hospital discharge such every bit home care services.
In addition, the case management plan of care y'all develop identifies outcomes that are measurable and doable within a manageable time frame and that utilize evidenced-based standards and care guidelines. You finalize the Planning phase (i.e., development of a final case direction plan of treat your client/support system) after you have received authorization for the health and human services from your client'southward payor source and after the services and resources needed have been identified.
The Implementing (Care Coordination) Phase
The Case Management Process: Implementing (Care Coordination)
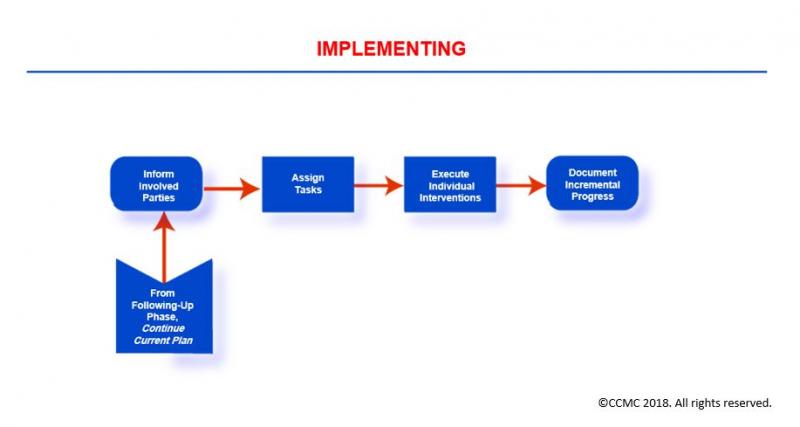
View larger image
Click here to view map key for image
The Implementing phase centers on the execution of the specific case management activities and interventions that are necessary for accomplishing the goals set along in your client'southward example management plan of intendance. This is unremarkably known as care coordination.
During this phase, you as the case manager organize, secure, integrate, and change (equally needed) the health and human being services and resources necessary to meet your client'south needs and interests. You also share key information on an ongoing basis with your client and customer'southward back up arrangement, the healthcare providers/clinicians you are collaborating with, your client's wellness insurance company/payor, and the representatives of customs-based agencies you lot have engaged or volition be engaging in the customer's care and case management plan.
The Post-obit-Upward Phase
The Case Management Process: Following-Up
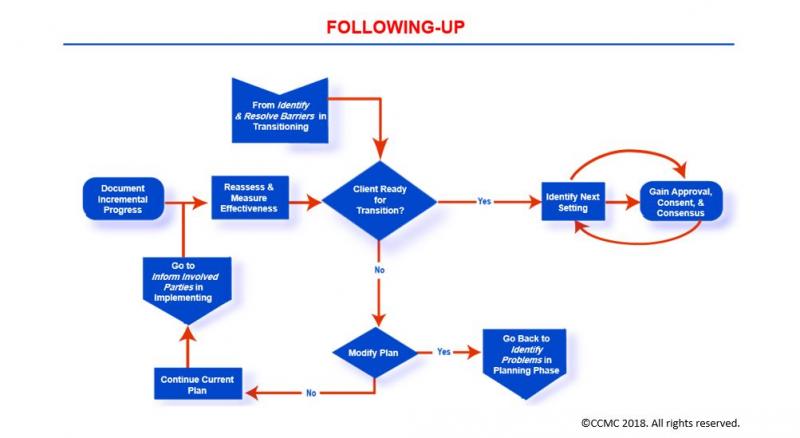
View larger image
Click here to view map key for image
The Following-Upwards stage focuses on the review, evaluation, monitoring, and reassessment of a client's health status, needs, power for self-intendance, knowledge of condition and treatment regimen, and outcomes of the implemented treatments and interventions. Here your chief objective is to evaluate the appropriateness and effectiveness of your customer'southward case management plan and its effect on your client's wellness condition and care outcomes.
During this phase, you:
- Gather sufficient information from all relevant sources
- Share data with your client, client's support system, healthcare providers, and others as advisable Document in your client's wellness record the findings, modifications yous may have fabricated to your client's case direction plan, and recommendations for intendance
- May echo these activities at frequent intervals and as needed
- Following-Upwards may indicate the demand for a modest modification or a complete alter in the case direction plan of care. You lot utilize this phase equally an opportunity to identify such needed revisions.
The Transitioning (Transitional Intendance) Phase
The Instance Management Process: Transitioning (Transitional Intendance)
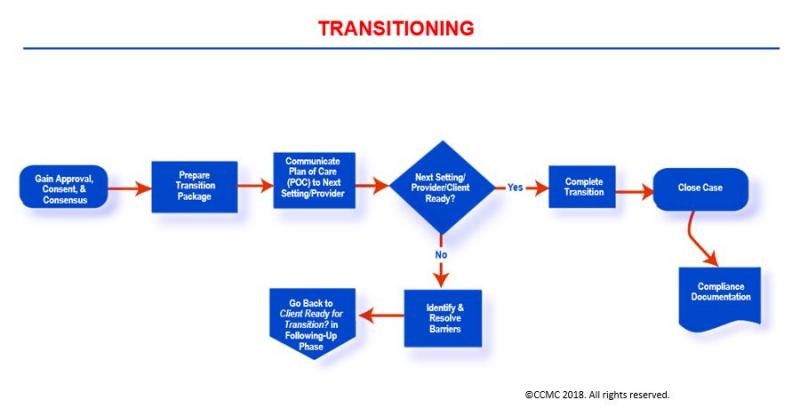
View larger image
Click here to view map key for prototype
The Transitioning phase focuses on moving a client across the health and homo services continuum or levels of care depending on the client'due south health condition and the needed services/resources.
During this phase, you as the case manager prepare your client and client'southward support arrangement either for discharge from the current intendance setting/facility to dwelling or for transfer to some other healthcare facility or a community-based clinician for further intendance. These activities are commonly known today equally transitional care or transitions of care. In order to maintain continuity of care, you lot apply this phase's activities to completely execute your client's transition to the adjacent level of care. You ensure your client's safe transition through careful communication with key individuals (including sharing of necessary information) at the next level of care or setting, your customer and client's support system, and other members of the healthcare team.
Additionally, you may:
- Educate your client about mail service-transition care and needed follow-up
- Summarize what happened during an episode of care
- Secure durable medical equipment (eastward.g., glucose meter, scale, walker) and transportation services (if needed) for your customer
- Communicate these services to your client, your customer'due south support system (such as caregiver), and to key individuals at the receiving facility or abode care agency (if applicable) or those individuals bold responsibility for your client'southward care mail transition
The Communicating Post Transition Phase
The Case Management Process: Communicating Mail Transition
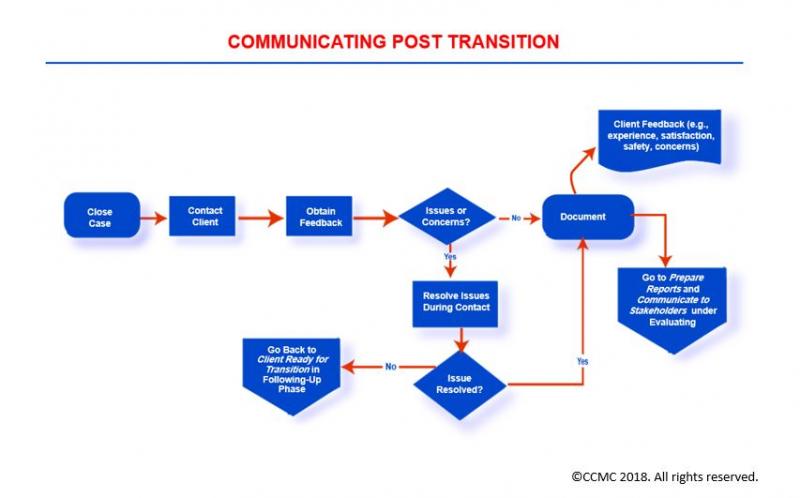
View larger image
Click here to view map cardinal for image
The Communicating Post Transition phase involves communicating with a client/support system for the purpose of checking on how things are going mail service transition from an episode of care.
As the instance manager during this stage, you lot enquire most your client's comfort with self-care, medications intake, availability of the mail service-transition services you may have arranged for (e.g., visiting nurse services), and presence of any issues or concerns. You also may solicit feedback regarding your customer's feel and satisfaction with services during the care episode.
During this phase, you:
- Follow upwards on the issues and problems y'all identify during the mail service-transition communication
- Seek resolution for the bug you identify
- Depending on the event or concern you have identified, you may engage other healthcare professionals to accomplish resolution
- Written report the feedback yous gather during the communication to key stakeholders such as payors and providers of care
The Evaluating Stage
The Case Management Process: Evaluating
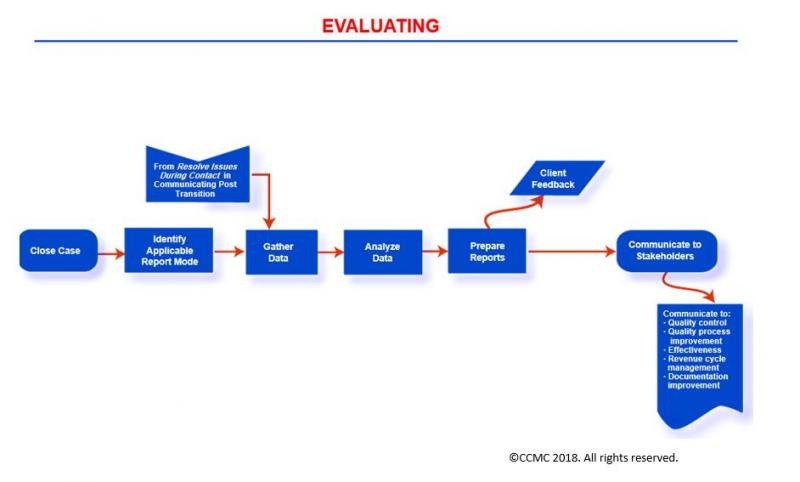
View larger image
Click here to view map key for paradigm
The Evaluating stage calls for measuring the results of implementing the client'southward example management program of care (e.g., the objectives, goals, treatments and interventions, and return on investment) and their consequence on a customer's condition. In this evaluation, you focus on several types of outcomes of care:
- Clinical
- Financial
- Quality of life
- Feel and satisfaction with intendance
- Concrete functioning
- Psychosocial and emotional well-being
- Self-intendance direction ability and health engagement
- Knowledge of wellness status and programme of care, including medications management
During this phase, y'all as the case manager generate outcomes reports such as case summary, quality, cost/billing, satisfaction, outcomes, toll-benefit analysis, and return on investment. You also communicate the findings or disseminate the reports to key stakeholders such as government agencies (east.g., Centers for Medicare & Medicaid Services), the leadership team, client, payor, providers of care, employers, interdisciplinary team members, risk management staff, quality improvement squad members, and others as accounted advisable.
Essential Domains of Case Management Noesis
Although case managers do in a diverseness of care settings and are from varied backgrounds, the Committee has now defined six essential knowledge domains that encompass the realm of case direction work and that apply to all intendance settings, wellness disciplines, and professional person backgrounds. Each domain is further organized into subdomains.
| Domain | Subdomains |
|---|---|
| Care Delivery and Reimbursement Methods |
|
| Psychosocial Concepts and Support Systems |
|
| Rehabilitation Concepts and Strategies |
|
| Ethical, Legal, and Practice Standards |
|
| Quality and Outcomes Evaluation and Measurement |
|
| Professional Evolution and Advancement |
|
Care Commitment and Reimbursement Methods
The Care Delivery and Reimbursement Methods domain consists of cognition associated with the Case Management Process, systems of care provision, resource, and skills needed to ensure the constructive and efficient commitment of safe, quality health and human services to clients/support systems. This domain as well includes noesis of reimbursement methods, funding sources, allocation of services and resource, and payor systems and concepts such as utilization review and management procedures.
Applying such cognition in the execution of your role and responsibilities as case manager enhances your performance and improves your productivity, which so ultimately results in enhanced care outcomes for both your client and employer (healthcare organization) alike.
Success in your case manager's office requires the work of a team: the client, the client's support system, and the healthcare and service providers, including payor representatives and other clinicians.
The Example Management Team
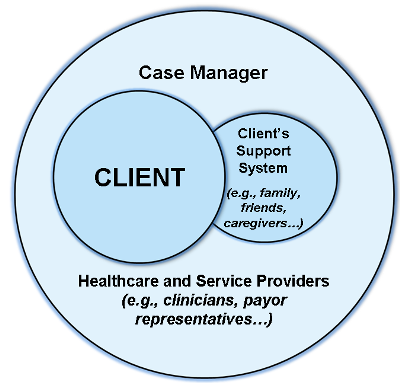 © CCMC 2018. All rights reserved.
© CCMC 2018. All rights reserved.
View larger paradigm
The Care Delivery and Reimbursement Methods domain also focuses on knowledge associated with case management administration and leadership, with plan blueprint and structure, with roles and responsibilities of case managers in various settings, and with skills of case managers (e.thousand., advice, problem solving, disharmonize resolution, resilience, and others).
Additionally, knowledge in this domain is associated with various healthcare delivery systems and models across the continuum of health and human services and case managers' practice settings. It includes knowledge of case management models, concepts, processes, services, and resources. Moreover, this domain addresses other topics such every bit levels of intendance, transitions of care, and collaboration among the various people involved in intendance such as the clients themselves, their support systems, multi-specialty care providers, community agencies, and payors.
Psychosocial Concepts and Support Systems
The Psychosocial Concepts and Support Systems domain consists of knowledge associated with the function clients' cultures, values, beliefs, social networks, and support systems play in clients' health and well-being, including health behavior and lifestyle. This domain also focuses on the impact of socioeconomic classes on clients' health conditions, ability for cocky-care management, health appointment, health literacy and numeracy, and adherence to treatment regimen.
Additionally, this domain includes knowledge of the case director's role in addressing bug of underinsurance or lack of insurance, clemency intendance, clients' education regarding health condition and treatment options, counseling and psychosocial back up, and clients' abode environments and living arrangements.
Rehabilitation Concepts and Strategies
The Rehabilitation Concepts and Strategies domain consists of knowledge associated with clients' physical and occupational health and functioning, including catastrophic case management, workers' bounty, vocational and disability concepts, strategies, and resources.
This domain besides includes cognition of life care planning, roles and skills of various healthcare providers in rehabilitation care settings, render-to-work concepts and strategies, types of rehabilitation settings/facilities, and use of assistive devices or durable medical equipment for rehabilitation and vocational purposes. In addition, this domain includes regulations pertaining to rehabilitation.
Quality and Outcomes Evaluation and Measurement
The Quality and Outcomes Evaluation and Measurement domain consists of knowledge associated with quality management, accreditation standards, care quality and safety, demonstrating return on investment, and cost-effectiveness. In add-on, this domain includes demonstrating the value of case management, case load adding, tools such as case management plans of intendance, and regulations related to instance management.
Ethical, Legal, and Practise Standards
The Ethical, Legal, and Do Standards domain consists of knowledge about the instance manager'south role as client advocate, and legal and ethical issues relevant to case management practice. This domain also focuses on:
- Codes of ideals and professional conduct for case managers
- Take chances management
- Regulatory and legal requirements
- Upstanding practices and principles
- Privacy and confidentiality
- Overall standards of case management practice
- Utilize of standards and guidelines in the management of clients' intendance
- Strategies for ethical and legal practice
Professional Development and Advancement
The Professional person Development and Advocacy domain consists of knowledge associated with the roles and responsibilities of case managers in articulating, advancing, and demonstrating the value of case direction practice. It also includes topics such as case managers' involvement in scholarship activities (eastward.g., writing for publication, public speaking, inquiry and utilization of testify, training and education, and curriculum development), health or public policy piece of work, accountability for ongoing education or learning, maintaining necessary skills and competencies for effective performance, engagement in practice innovation, and mentoring other case managers.
Which Tool Is Often Used By Case Managers?,
Source: https://cmbodyofknowledge.com/content/introduction-case-management-body-knowledge
Posted by: hansonlins1970.blogspot.com


0 Response to "Which Tool Is Often Used By Case Managers?"
Post a Comment